Mark Bertolini has helped Oscar Health move toward profitability after taking over as CEO of the health insurer a year ago. Now, he says the company’s next phase of growth and profitability will focus on tapping into the employer market.
That effort will include “going after the 71 million lives that are in small group and middle market employers, where most employees are over-insured to take care of the few sick people in the group to get a level premium,” Bertolini explained, ahead of the company’s investor day Friday.
“We have a huge opportunity to create a whole new market,” he added.
It’s not a new concept. When Affordable Care Act exchanges launched 10 years ago, analysts predicted employers would abandon the complexities of buying group coverage and adopt individual coverage health reimbursement arrangements, or ICHRAs, giving workers cash to buy their own ACA plans.
Bertolini says the market never took off because insurers were not focused on keeping costs down for employers or their workers.
“What we’re now going to do is put plan designs in and underwrite the group. So we get the employees to the right plans — like an ultimate flexible benefit plan,” he said.
Moving into the employer market is part of Oscar’s strategy to expand its membership from 1.5 million to roughly 4 million by 2027.
Ahead of its analyst day presentation, the company set a target of achieving approximately 20% annual revenue growth over the next three years and earnings of $2.25 per share in 2027.
Focus on PBM contracts
After serving as CEO of Aetna for eight years, Bertolini has deep knowledge of how large insurers and pharmacy benefit managers operate. Earlier this year, he likened his role at Oscar to being on a pirate ship ready to disrupt big Spanish galleons laden with gold.
Last year, he helped Oscar negotiate more favorable terms on its pharmacy benefit management, or PBM, contract with CVS Health’s Caremark division, which he says has helped Oscar control medical costs on its plans.
Oscar Health’s contract with CVS Caremark runs through 2026.
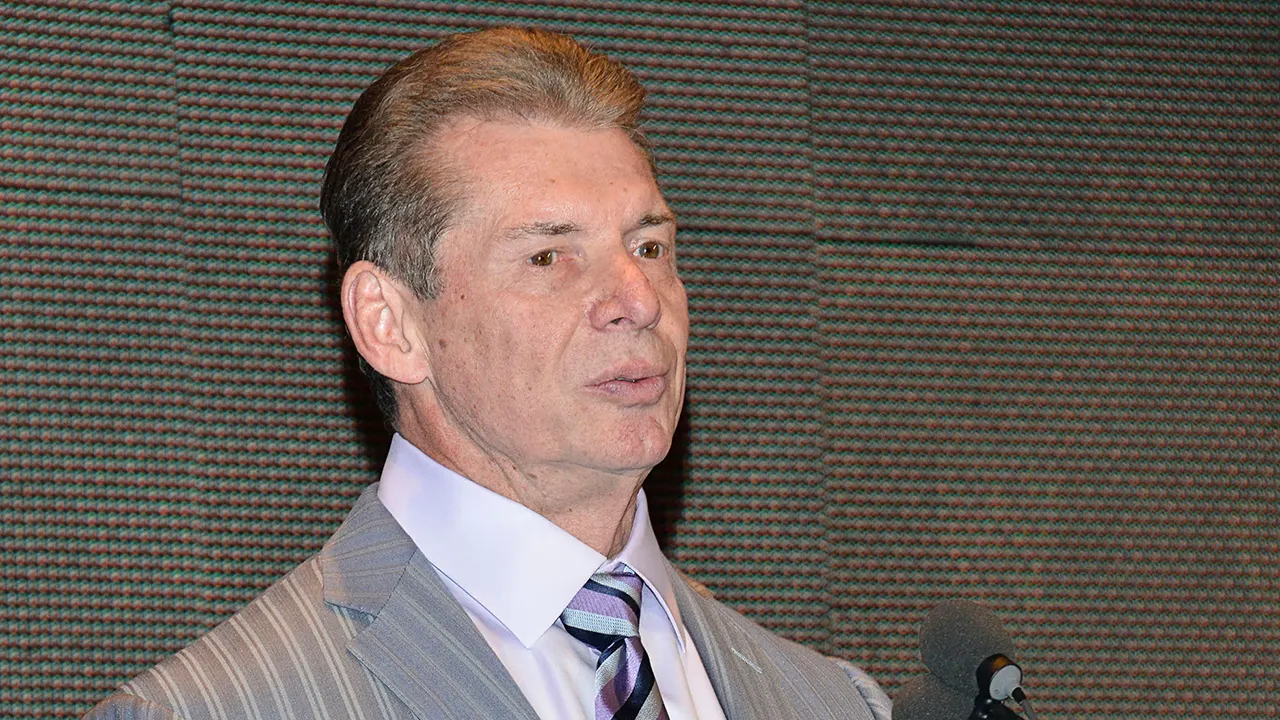
Mark Bertolini speaking at the CNBC Evolve New York event on June 19. 2019.
Astrid Stawiarz | CNBC
Next year, Bertolini will be watching how health insurer Blue Shield of California implements its potentially disruptive PBM model.
Blue Shield contracted with a smaller PBM firm for the bulk of its drug benefits in an attempt to rein in costs for its members. It will use Mark Cuban’s Cost Plus Drugs and Amazon Pharmacy as its preferred pharmacy networks starting in 2025.
“I think the PBM model is played out,” Bertolini said. “They need to start being legitimately straightforward with the customer base and saying, we’re going to pass on all the [savings] that we’ve been able to create with the size of our organization directly to you. If they make that leap, either through insurance premiums, or through the pharmacy itself, then I think they can stick around.”
The three major U.S. PBMs — CVS’s Caremark, Cigna’s Express Scripts and UnitedHealth Group’s Optum Rx — have seen their businesses come under increasing regulatory scrutiny. Over the last year, all three have launched more transparent pricing models for insurance and employer clients.