It may still feel like summer, but the fall is quickly approaching — along with the risk of seasonal viruses.
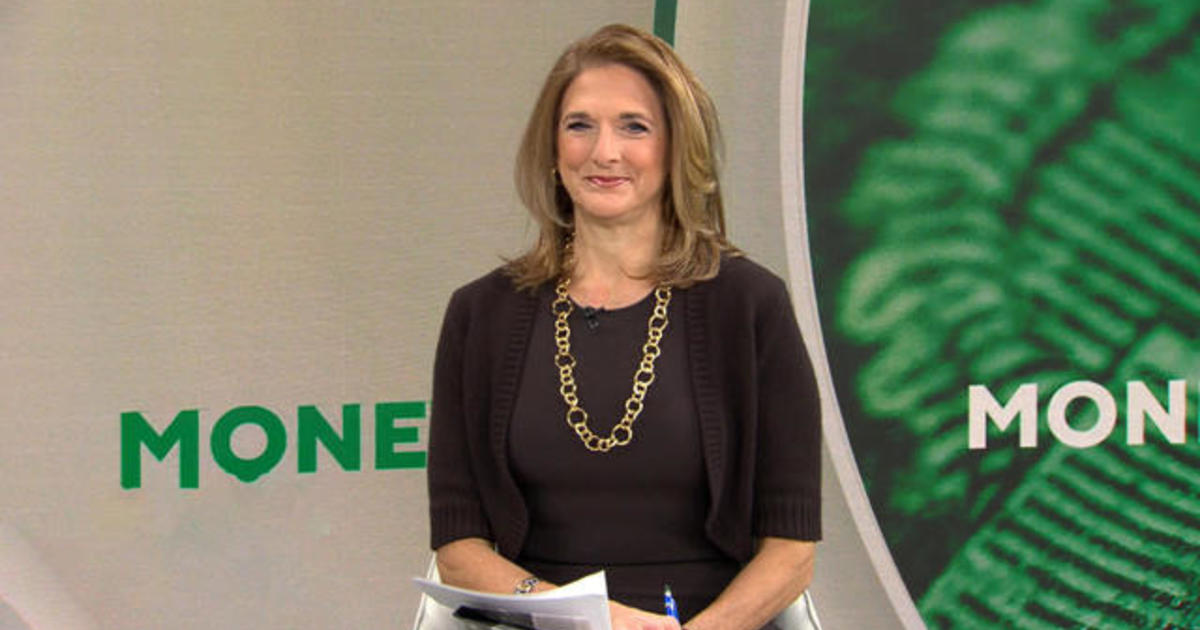
On “CBS Mornings” Monday, Dr. Céline Gounder, a CBS News medical contributor and editor-at-large for public health at KFF Health News, shared what you need to know about protecting yourself from COVID-19, the respiratory illness RSV and the flu — three infections that raised concerns last winter about the threat of a “tripledemic.”
The recommendations are especially important for those at high risk, including people who are elderly, pregnant or have chronic health conditions.
Here’s what you need to know:
Is there an RSV vaccine?
There are a few prevention tools for RSV, or respiratory syncytial virus, an illness that typically causes cold-like symptoms but can sometimes be severe, especially for infants and older adults.
“(There’s) a vaccine for the elderly for people 60 and up,” Gounder says. “For this one, we recommend you talk to your health care provider and see if they recommend it for you.”
There is also a new kind of immunization to protect babies from RSV that was recently approved by the Food and Drug Administration. The drug, nirsevimab, is one of two new options doctors hope could soon prevent many cases of the illness, which is the leading cause of hospitalization facing American infants. Drugmakers AstraZeneca and Sanofi will market it under the brand name Beyfortus.
As Gounder explains, it isn’t a vaccine but a monoclonal antibody shot.
“This is to protect young infants who are very high risk for severe RSV,” Gounder says. “If you have an infant who is 8 months or less, all infants are recommended. For infants eight to 19 months, it really depends on if they were born prematurely or have other risk factors.”
Previously, parents and doctors only had one option to shield some babies from RSV: monthly injections of palivizumab, an antibody drug which is recommended for use in infants and young children with conditions that put them at higher risk.
Do I need a COVID booster?
“We have seen a 10% increase in hospitalizations over the last few weeks, but 10% of a very small number is still a very small number,” Gounder says. As summer comes to a close, there’s concern that cases could rise more sharply in the fall and winter.
There will be an updated vaccine formula with boosters available to add protection against recent variants.
“Just because you’ve been infected does not mean you have full protection,” Gounder noted. “We’re still seeing much higher rates of hospitalization and death, for that matter, among people who remain unvaccinated.”
With that in mind, everyone age 6 months and older is eligible for a booster shot this fall. It’s especially important for those at high risk, Gounder says. This includes:
- Elderly people
- Nursing home residents
- Pregnant women
- Immunocompromised people
- Patients with lung and heart conditions
If you don’t fit into these high-risk groups, the choice to boost is up to you, Gounder says.
“Some people feel more concerned. Are you the person who gets the flu shot every year? You’re probably going to want to get that COVID shot,” she says. “If you’ve already been fully vaccinated, it’s less important for that young, healthy group.”
When should I get the flu shot?
Because of the lingering effects social distancing and masking has had on shifting timelines, experts predict flu season will start a bit early again this year, Gounder says, so don’t wait too long to get your flu shot.
“Big picture I would say September, October,” Gounder advises. “Whenever you’re able to get in to get your flu shot is a good time to do it.”
During last year’s flu season, the flu shot provided “substantial protection” for all age groups, including elderly and immunocompromised populations, according to data the Centers for Disease Control and Prevention reported earlier this year.
-Alexander Tin contributed to this report.